Key Takeaways:
-
Menopause Made Clear: Understanding the menopause timeline helps decode symptoms and prepares you for changes in cycle length, flow, mood, temperature regulation, and bladder health.
-
Menopause Journey Explained: The stages of menopause include perimenopause, menopause, and postmenopause, each with unique symptoms and strategies for management.
-
Your Menopause Blueprint: Key factors like genetics, lifestyle, and medical history influence the timing of menopause and highlight the importance of consulting with healthcare providers for tailored, effective management.
Menopause doesn’t arrive overnight—it’s a gradual process that unfolds over several years. Officially, menopause is marked by 12 consecutive months without a period, typically occurring between ages 45–55.(World Health Organization). But most women experience changes before this, during perimenopause, which can start in the early 40s (or even late 30s) and last from a few months to almost a decade. Menopause is a normal evolution involving the permanent end of menstrual cycles due to the cessation of the production of reproductive hormones from the ovaries for at least 12 consecutive months.(National Library of Medicine)
Perimenopause brings a range of symptoms: irregular cycles, heavier or lighter flow, hot flashes, mood changes, disrupted sleep, and sometimes bladder leaks due to shifting hormones and pelvic floor changes. These signs signal your body’s transition towards menopause and are completely normal, though sometimes surprising. It is a disruptive process that can last for over a decade and causes symptoms in a majority of women.(JCEM)
Preparation is key: track changes in your cycle, prioritize sleep, eat a balanced diet, stay active, and consider reliable support products—like Saalt’s leakproof panties—for comfort and confidence. Staying informed helps you feel more in control through each phase: perimenopause, menopause, and postmenopause.
Everyone’s menopause journey is unique, but you don’t have to navigate it alone. By recognizing early signs and equipping yourself with practical solutions, you can ease the process and take charge of your health and well-being through this natural transition.
Menopause 101: Understanding the Transition
Menopause is a gradual transition, not a sudden switch. Understanding its stages can empower you to navigate symptoms and self-care with confidence.
-
Perimenopause: Often starting in your 40s (sometimes late 30s), hormone levels fluctuate, causing changes in your cycle, mood, and body. This phase typically lasts 4–8 years.
-
Menopause: Diagnosed after 12 months without a period, usually around age 51. Symptoms like hot flashes and night sweats may peak during this time.
-
Postmenopause: Begins after one year without a period. Some symptoms fade, but bone health, heart health, and pelvic floor changes remain important.
You may notice:
-
Irregular cycles, heavier or lighter periods
-
Hot flashes, night sweats, and sleep disruptions
-
Mood swings, anxiety, and brain fog
-
Pelvic floor and bladder symptoms, vaginal dryness
-
Slower metabolism and body composition shifts
To prepare and support your health:
-
Find a clinician who listens and specializes in menopause care
-
Track symptoms, sleep, and cycles
-
Focus on strength training, nutrition, and hydration
-
Consider pelvic floor exercises and balance work
-
Explore treatment options, including hormone therapy, with your provider
Bottom line: Menopause typically starts with perimenopause in your 40s. Recognizing changes early—and partnering with supportive providers—can make the transition smoother and help you thrive postmenopause.
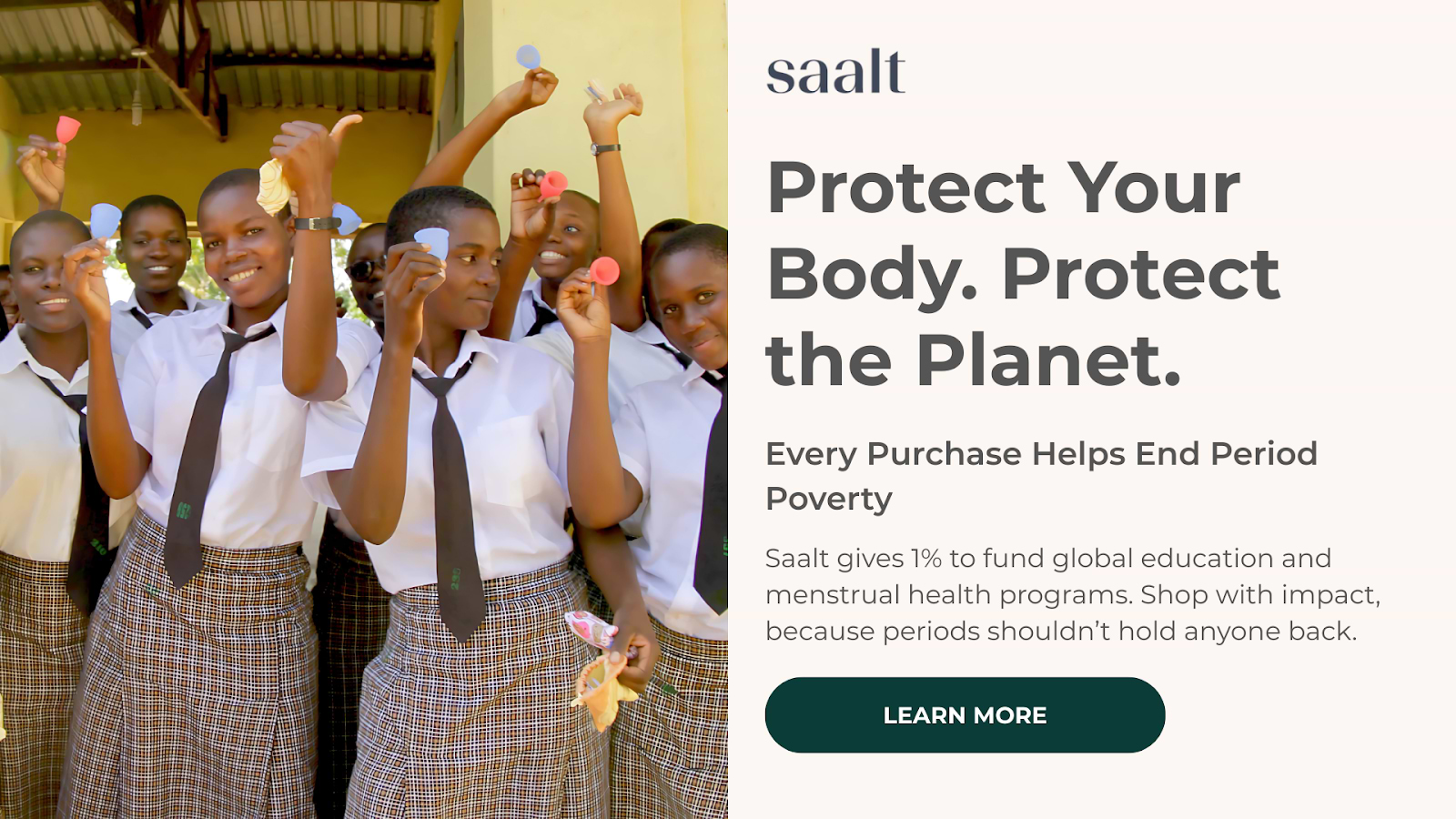
Stay Active, Leak-Free, and Confident with SaaltYou don’t have to white-knuckle your way through perimenopause and menopause. If you’re asking “when does menopause start?” you’re already ahead—now set yourself up to feel prepared on every run, meeting, and midnight bathroom trip. Saalt’s leakproof essentials are built for real life and all its curveballs. · Choose your coverage: From light liners to heavy-absorbency underwear, pick styles that handle bladder leaks, discharge, and period flow—without bulk. · Feel-good materials, no compromises: Saalt underwear is made without PFAs in the finishing process and engineered for breathable, all-day comfort. · Sustainably smart: As a certified B Corp donating 1% to impact programs, Saalt helps reduce waste while expanding period equity worldwide. · Mix and match your toolkit: Pair Saalt’s premium reusable menstrual cups and discs with leakproof underwear for overnight confidence and on-the-go back-up. · Built for every chapter: Teen to postpartum to perimenopause to beyond—Saalt supports you at every stage so you can keep moving. Ready to stop planning your day around bathrooms? Make the switch that frees up your brain—and your calendar. · Explore Saalt Leakproof Underwear · Get 10% off your first order when you subscribe to emails Take control of your timeline. Saalt’s got the rest. |
The Three Stages: Perimenopause, Menopause, Post-Menopause
Menopause unfolds in three distinct stages: perimenopause, menopause, and post-menopause. Each comes with its own timeline and symptoms, but understanding them can help you manage this transition with confidence.
Perimenopause: The Build-Up
Usually starting in your 40s (sometimes late 30s), perimenopause features hormonal fluctuations and unpredictable cycles. Common symptoms:
-
Irregular periods
-
Hot flashes/night sweats
-
Insomnia, mood changes, brain fog
-
Vaginal dryness, shifting libido, bladder changes
Perimenopause can last 2–10 years. Tracking symptoms, maintaining sleep, strength training, and nutrition support are key. Consult a clinician if symptoms interfere with life.
Menopause: The Turning Point
Menopause is reached when you go 12 consecutive months without a period, typically around age 51. Symptoms may include continued hot flashes, vaginal/urinary changes, and mood shifts. Bone density and cardiovascular risks start to rise at this stage.
-
Maintain regular exercise
-
Screen for bone health
-
Discuss hormone therapy options with your doctor
Post-Menopause: The New Normal
After a year without a period, you’re officially post-menopausal. Symptoms may stabilize, but hot flashes or vaginal dryness might persist. The focus shifts to:
-
Health screenings (bone, heart, pelvic exams)
-
Nutrition for longevity
-
Stress management, staying active, and social connections
Knowing these stages empowers you to support your body at every turn.
Average Age and Factors That Influence Timing
Menopause typically arrives around age 51 in the U.S., but the transition (perimenopause) often begins in the mid-to-late 40s and can last up to 10 years. Timing varies widely: some women reach menopause in their early 40s, while others do not until their mid-50s. While there’s no fixed schedule, several key factors influence when menopause occurs:
-
Genetics: Family history provides the best clues to timing.
-
Smoking: Leads to menopause up to two years earlier.
-
Reproductive history: Earlier menarche or irregular cycles may influence timing.
-
Health conditions: Autoimmune disorders and certain cancer treatments can cause earlier onset.
-
Surgery: Removing both ovaries causes immediate menopause.
-
Body weight: Lower body fat may be linked to earlier menopause.
-
Ethnicity: Timing and symptoms can differ among racial and ethnic groups.
-
Environment & stress: Chemical exposures and chronic stress impact hormonal balance and may affect menopause age.
Most women notice subtle changes in their late 30s or early 40s, such as cycle variability and mild symptoms. This intensifies in the mid-to-late 40s, with irregular periods and possible hot flashes. When you go 12 months without a period, you’ve reached menopause, usually between 50 and 52. If menopause happens before 40, or symptoms are severe, consult your healthcare provider to rule out underlying conditions.
Early or Late Onset: When to Consult a Provider
Menopause timing varies—most reach it around 51, but perimenopause can start sooner or later. If you’re wondering when to check in with a healthcare provider, here are key signs:
-
Before age 40: Menopausal symptoms this early can signal premature ovarian insufficiency. Early evaluation is essential for long-term bone and heart health.
-
Between 40–45: Early symptoms may be normal but should be discussed—other factors like thyroid issues can mimic menopause.
-
If still menstruating after 55: Check in to rule out fibroids, endometrial changes, or medication effects.
-
Unusual bleeding: Any bleeding after 12 months without a period, significantly heavier flow, or bleeding between periods needs prompt evaluation.
-
Disruptive symptoms: Chronic insomnia, severe mood swings, brain fog, or persistent joint pain are all valid reasons to seek help.
-
Relevant history: Family history of early menopause, autoimmune conditions, or prior chemotherapy are red flags for early monitoring.
Prepare for your appointment by logging symptoms, listing medications, and clarifying your health goals. Your provider may order hormone-related labs, recommend imaging for abnormal bleeding, or suggest treatments like cognitive behavioral therapy, nonhormonal medications, or hormone therapy tailored to your needs.
Bottom line: If your menopause journey feels too early, too late, or just off, talk to a provider. Early conversations ensure you get answers—and the support you need to feel your best.
Hormonal Changes Behind the Symptoms
The hallmark symptoms of perimenopause and menopause—hot flashes, irregular cycles, mood swings, sleep issues—are all tied to changing hormone levels, chiefly estrogen and progesterone, with testosterone playing a minor role.
Estrogen is the main driver, and it doesn’t just gradually decline. Instead, it fluctuates sharply, causing irregular periods, hot flashes, and night sweats as your body’s internal thermostat gets thrown off. Progesterone, which helps regulate mood and sleep, drops more steadily when ovulation becomes unpredictable, often resulting in sleep disruptions and heightened anxiety or PMS-like moods. Testosterone declines more gradually, but loss of it can sap energy and lower libido.
These hormone shifts explain why periods get unpredictable; why heat surges, sweats, and chills can hit suddenly; and why mood and focus may nosedive. Lower estrogen also causes thinning vaginal tissue and urinary changes, sometimes leading to discomfort and more frequent infections. Sleep loss is common, as falling progesterone disrupts natural sleep rhythms and night sweats keep you awake.
Counteracting these effects involves tracking your symptoms, focusing on strength training and regular movement, supporting sleep habits, and eating for stable blood sugar and bone health. If symptoms affect your quality of life, talk to a healthcare provider about menopause-specific treatments.
The bottom line: Understanding that these symptoms stem from hormonal changes during perimenopause and menopause helps you adapt proactively—so you can protect your well-being and work with your body’s new rhythm, not against it.
The Bottom Line
Menopause isn’t a cliff you fall off—it’s a timeline, with milestones that are worth understanding so you can plan, adapt, and keep living on your terms. From the first whispers of perimenopause to the final period and beyond, your body is signaling change, not defeat. Track your symptoms, loop in your healthcare provider, and build your toolkit: nutrition that supports bone and heart health, movement that keeps you steady and strong, sleep routines that actually stick, and leak protection that lets you stay active without the what-ifs.
If bladder leaks show up (and for many, they do), you’re not alone—and you’re not stuck. Saalt Leakproof underwear offers breathable protection in multiple absorbencies and styles, so you can lift, jog, laugh, and live without calculating the nearest bathroom. It’s sustainable, reusable, and made to keep pace with you—whether you’re juggling kids, recovering postpartum, or navigating hot flashes on a crowded train.
Menopause is personal, but it doesn’t have to be isolating. Equip yourself with knowledge, choose products that respect your body and the planet, and give yourself credit for every day you show up—comfortable, prepared, and unapologetically you. Saalt’s here to make the leaks a non-event, so you can focus on everything else.
Read Also:
FAQs About Menopause
What is menopause?
Menopause is a natural biological transition that marks the end of menstrual cycles. Clinically, it’s confirmed after 12 consecutive months without a period, not caused by pregnancy, illness, or medication. It’s driven by declining ovarian function and lower levels of estrogen and progesterone. Menopause isn’t a sudden cliff—it’s a progression that includes perimenopause (the lead-up), menopause (the milestone), and postmenopause (the long-term phase after). While it can bring symptoms like hot flashes and bladder leaks, it’s also a chance to recalibrate your routine, advocate for your health, and find products that help you stay active and comfortable.
When does menopause typically start?
Most women reach menopause between ages 45 and 55, with the average around 51. The transition often starts earlier with perimenopause—usually in the mid-to-late 40s, but it can begin in the late 30s for some. Factors that can shift timing:
-
Genetics: If your mother or sisters experienced early or late menopause, you might, too.
-
Smoking: Often linked to earlier onset.(Science Direct)
-
Health history: Autoimmune conditions, chemotherapy, radiation, or ovary-removal surgery can accelerate or trigger menopause.
-
Ethnicity and BMI: Can influence symptoms and timing. If you’re wondering “when does menopause start,” track cycles, note changes, and bring a symptom log to your provider for a personalized picture.
What are the early signs of menopause?
Early signs typically surface in perimenopause and can ebb and flow. Common signals include:
-
Cycle changes: Shorter or longer cycles, heavier or lighter flow, unexpected spotting.
-
Vasomotor symptoms: Hot flashes, night sweats, flushes that come in waves.
-
Sleep disruption: Trouble falling or staying asleep, often tied to night sweats.
-
Mood shifts: Irritability, anxiety, low mood, or brain fog.
-
Vaginal and urinary changes: Vaginal dryness, discomfort during sex, more frequent UTIs, and stress incontinence or bladder leaks.
-
Body changes: Breast tenderness, joint aches, new headaches, or changes in hair/skin.
-
Libido fluctuations: Desire may go up or down. If bladder leaks creep in during workouts, sneezes, or long runs, you’re not alone—pelvic floor shifts and lower estrogen can play a role. Supportive routines, pelvic floor exercises, and leakproof underwear can make an immediate difference while you explore longer-term solutions with your provider.
How long does menopause last?
The milestone of menopause itself is one day—the 12-month mark without a period. The broader transition is longer:
-
Perimenopause: Typically 4–8 years, though it can be shorter or longer.
-
Postmenopause: Begins after that 12-month mark and continues for the rest of life. Some symptoms, like hot flashes, may resolve within a few years; others, like vaginal dryness or bladder sensitivity, can persist without treatment. Managing the long arc often means a layered plan: lifestyle shifts (sleep, strength training, pelvic floor work, nutrition), targeted therapies (lubricants/moisturizers, vaginal estrogen, or systemic hormone therapy when appropriate), and practical tools that make day-to-day life easier—like Saalt Period Underwear in a range of absorbencies to handle bladder leaks, spotting, or light flow. Saalt is made without PFAs in the finishing process, comes in multiple styles and sizes, and is designed to help you stay active without the backup plans.
Sources:
-
The Journal of Clinical Endocrinology and Metabolism. (2020, October 23) The Menopause Transition: Signs, Symptoms, and Management Options. https://academic.oup.com/jcem/article/106/1/1/5937009
-
National Center for Biotechnology Information. (2023, December 21) Menopause. https://www.ncbi.nlm.nih.gov/books/NBK507826/
-
Science Direct. (2023, September 14) Menopause – Biology, consequences, supportive care, and therapeutic options. . https://www.sciencedirect.com/science/article/pii/S0092867423009054
-
World Health Organization. (2024, October 16) Menopause. https://www.who.int/news-room/fact-sheets/detail/menopause
tags: Leakproof Underwear, Menstrual Cup, When Does Menopause Start: Timeline & Preparation - Saalt,





![hanky panky+ [powered by Saalt] French Brief](https://sfycdn.speedsize.com/580f55fb-12e3-4e00-8f82-e44e2431f676/https://saalt.com/cdn/shop/files/SW-HP-PDP-Portrait-French-Brief-Navy-Front_medium.jpg?v=1762200243)




